| This web site was created to raise public awareness of treatment options for binocular vision impairments, such as amblyopia ("lazy eye") and strabismus (wandering eye, wall-eyes, crossed-eyes Crossed Eyes, Wandering Eye, Deviating Eyes, Esotropia, Exotropia, Esophoria, Exophoria, Hyperphoria, Hyperopia, Astigmatism, Alternating Esotropia), Convergence Insufficiency, Double Vision, Diplopia, Nystagmus, Loss of Depth Perception, Poor Binocular Vision, Accommodative Problems, Tracking Problems, Loss of Depth Perception, Loss of stereoscopic vision and/or binocular fusion, Learning Related Vision Problems. |
What is Binocular Vision?
BINOCULAR: Of or involving both eyes at once.
BINOCULAR VISION: Vision wherein both eyes aim simultaneously at the same visual target; vision wherein both eyes work together -- simultaneously, equally and accurately -- as a coordinated team.
Healthy binocular vision produces important visual perceptual skills which are part of normal human vision: binocular depth perception and stereopsis.
STEREOPSIS: (stereopsis or stereoscopic vision) vision wherein two separate images from two eyes are successfully combined into one image in the brain.
Stereopsis is an aspect of "normal" healthy vision. Here's how it works. First, both eyes must be accurately aimed at the same target (that's binocular vision, but it's not yet stereoscopic vision!) Then, because the two eyes are located in different positions, each takes in a unique view from its own perspective. The two separate images are sent on to the brain for processing. When the two images arrive simultaneously in the back of the brain they are united into one picture. The combined picture appears three-dimensional (3-D) because it has the added depth dimension. That's stereo vision. Stereo vision gives you depth perception. For an illustrated definition, see the Stereo Vision page.
What is Binocular Vision Impairment?
A binocular vision impairment is any visual condition wherein binocular visual skills are inadequately developed. A comprehensive eye examination should include the testing of these important binocular visual skills:
| Tracking: the ability to move the eyes across a sheet of paper |
| Fusion: the ability to use both eyes together at the same time |
| Stereopis: binocular depth perception |
| Convergence: the ability of the eyes to move and work as a team |
| Visual Motor Integration: the ability to transform images from a vertical to a horizontal plane |
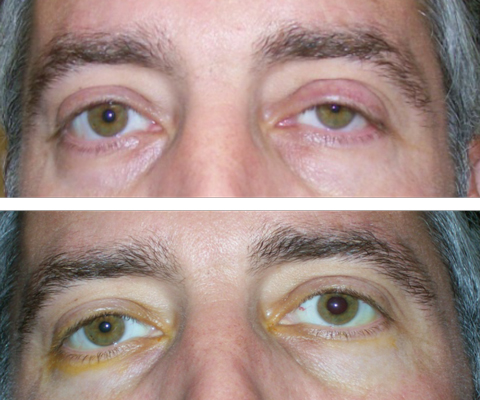
Binocular vision impairments often result in partial or total loss of stereoscopic vision and binocular depth perception. Conditions where the eye is obviously turned or crossed are commonly referred to with terms like "cross-eyed", "crossed-eyes", wall-eyes" or "wandering eyes". These binocular vision impairments are easily detected by others as all the observer needs to do is notice that both eyes do not aim in the same direction at all times. Some medical terms for these deviations or misalignments of the eye are strabismus, esotropia, exotropia, congenital strabismus, hereditary strabismus, pediatric strabismus, adult strabismus, accommodative esotropia, alternating esotropia, congenital esotropia, accommodative esotropia, esophoria, exophoria, exotropia, exotropic, esotropic, hyperphoria, hypophoria, hyperphoria, hypertropia. Other medical conditions which can contribute to poor binocular vision are anesmetropia, astigmatism, nearsightness, myopia, farsightedness, hyperopia, nystagmus, cerebral palsy, cataracts.
PLEASE NOTE: Some binocular vision impairments are not easily detected by parents, teacher or others because the turning or straying of the eye(s) is NOT obvious or consistent. Some eye turns are intermittent (they come and go) and/or they are not easily noticed by the untrained observer. A binocular vision problem is indicated, even when an eye turn is only occasionally visible. That's why early examination is so important.
Has your child been given different prescriptions for his or her two eyes? It is important to note that binocular vision is often impaired when the vision in the two eyes is significantly different or if one eye is higher than the other. The wearing of prescription glasses ONLY will rarely correct poor binocular vision.
Binocular vision impairments are more common than you may think. Just one type of binocular impairment, amblyopia ("lazy eye"), affects approximately 3% of the population. At least 12% of the population has some type of problem with binocular vision. Plenty of people are seeing the world with only one eye. They are monocular (one-eyed), not binocular (two-eyed). (Remember the monocles that people used to wear in the nineteenth century?)
Many monocular people can be rehabilitated with the help of Vision Therapy. They can become binocular and gain depth perception! children-special-needs.org seeks to call attention to binocular vision impairments and to educate parents and the public about treatment options. Many parents of children with these visual defects are not informed of all treatment options and are not gaining information about and access to Vision Therapy, a treatment option that offers a much higher success rate than eye muscle surgery.
What is Vision Therapy?
VISION THERAPY: (also known as vision training, visual training, visual therapy, eye training, behavioral optometry or orthoptic therapy):
Vision therapy can be described as physical therapy for the visual system which includes the brain and eyes. Through a series of progressive therapeutic procedures (eye exercises), patients develop or recover normal visual skills. Vision therapy is remarkably successful in rehabilitating all types of binocular vision impairments including amblyopia (lazy eye), strabismus, esotropia, exotropia, hyperphoria, or loss of binocular fusion due to hyperopia (farsightedness), myopia (nearsightedness) or astigmatism in one eye. In regards to the development or recovery of binocular vision, Vision Therapy is much more successful than surgery or glasses alone.
Who Can Benefit From Vision Therapy?
Patients of all ages can benefit from Vision Therapy. The nature of the therapy program varies with the condition treated. For example, a three year-old child with amblyopia, or "lazy eye", might have the better eye patched for a short period of time. An eight year old with strabismus "crossed eye", may require therapy for a period of a year to to gain BOTH cosmetic and visual benefits (the two eyes will appear straight AND will be used as a binocular team for normal vision). A 30 year-old computer programmer may require three to six months to solve a visual problem causing significant eye strain. A 30 year-old with strabismus who had two or more unsuccessful surgeries as a child might require two or more years of therapy. For information on patients with dyslexia, attention deficit disorder, and other conditions related to visual perception and information processing, see add-adhd.org.
Vision therapy can improve visual skills such as stereopsis, binocular coordination, binocular fusion, eye teaming skills, convergence, visual acuity, focusing skills, stereoscopic vision, depth perception, eye tracking, fixation skills, visual form discrimination, visual memory, hyperopia, and visual motor integration (balance, body coordination, hand-eye coordination).
Is Vision Therapy New?
Although Vision Therapy is currently an Optometric specialty, it is actually an outgrowth of orthoptics. Orthoptics, which literally means "straightening of the eyes", was introduced to this country by physicians in the late 1800's. As physicians became more focused on eyeglasses, medication , and surgery, the benefits of orthoptics were taught to fewer and fewer practitioners. However, optometrists in the mid 1900's took the best that orthoptics had to offer, and pioneered the development of Vision Therapy.
What's Involved In A Vision Therapy Program?
Patients typically come to the office twice weekly for 30 - 45 minutes each visit. In addition, homework is given to be done at home as reinforcement of what is learned during the office therapy sessions. Commitment to the therapy program, and maintaining a schedule of weekly visits, is important in the success of the program.
Can't my child just do the therapy at home?
Vision therapy programs are individualized for the patient, and careful guidance and frequent monitoring is required for success. When attempted by patients without guidance, poor visual habits may actually be reinforced. In addition, in-office Vision Therapy programs make use of specialty computer programs, regulated medical devices (such as lenses and prisms) and other tools which are not available for use in the home.
PLEASE NOTE: Vision therapy is NOT the Bates Method. The Bates Method was invented by W.H. Bates, an ophthalmologist who wrote Perfect Sight Without Glasses (New York, 1920). The eye procedures (eye exercises) employed in Vision Therapy are different from those of the Bates Method. Vision therapy involves a medically supervised program of therapeutic procedures (eye exercises). The techniques and technologies of Vision Therapy have been reviewed and developed throughout this century by doctors of optometry. In some cases, regulated medical devices (such as lenses and prisms) are used.
Will My Insurance Cover Vision Therapy?
Some of the better health insurance policies cover Vision Therapy. The answer to this question has absolutely no relationship to whether or not your insurance covers eye examinations, eyeglasses, or contact lenses. If and when it is covered, Vision Therapy would be viewed and paid more like physical therapy or occupational therapy. Managed care companies have been limiting payment on all types of licensed medical therapies. It is recommended that parents not allow insurance companies to make arbitrary decisions which prevent children from receiving necessary care. Note that Vision Therapy is very inexpensive and cost-effective when compared to surgical treatments.
How Long Does Vision Therapy Last?
When the program is complete, the benefits of Vision Therapy will last for a lifetime. Accurate focusing and the use of both eyes together efficiently is a reflex which, when conditioned, should operate effortlessly. Self-monitoring activities are prescribed at the end of each therapy program. Non-medical Vision Therapy, as related to visual perception, prepares children for a lifelong learning, and fills in gaps for many adults who have lost visual skills and abilities.
NO GUARANTEE OR WARRANTY IS STATED OR IMPLIED:
While Vision Therapy has been extremely effective for many individuals, no guarantee as to the effectiveness in any specific case is made by children-special-needs.org. Patient outcomes can vary widely from individual to individual, and as such, no warranty is stated or implied. |
Why Is Vision Therapy a Well-kept Secret?
- If the media would bring in the cameras more often, it might be a different story. Most of us have seen dramatic camera footage of a physical therapy patient learning to walk again after a traumatic event. In comparison, it's much more difficult to present a dramatic picture of a child learning to see. In the case of visual improvements, most of the action is happening inside the child's own brain and can't be picked up by the eye of a camera.
Orthoptics -- a part of Vision Therapy -- is practiced by both optometrists and pediatric ophthalmologists (orthoptics), but -- depending on the doctor you consult -- you or your family may never be told about either Orthoptics or Vision Therapy. There are many reasons for this, such as:
- The majority of pediatric ophthalmologists do not offer Orthoptics or Vision Therapy. Pediatric ophthalmologists are trained to be surgeons, not therapists. Their practices concentrate on the use of drugs and surgery to treat eye disease and trauma.
- The majority of optometrists, also, do not maintain active therapy practices. Optometrists who provide Vision Therapy are professional specialists who called themselves Behavioral Optometrists or Developmental Optometrists.
- Unfortunately for the patient, there are some territorial disputes between the two licensed professions of ophthalmology and optometry. This can lead to the patient not being referred elsewhere for the most effective treatment method. To understand the difference in practice between ophthalmologists and optometrists, see Choosing an Eye Doctor.
Many factors add up to the likelihood that you may not just stumble upon an eye doctor who offers Vision Therapy. To locate a qualified eye doctor who does provide Vision Therapy, go to the Referral Directory: Find a Pediatric Eye Doctor.
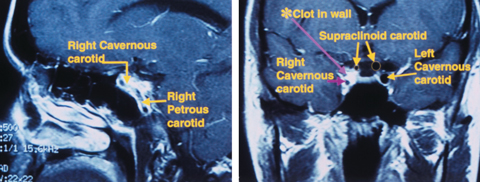
Is This an Eye Problem or a Brain Problem?
The visual system includes the brain as well as the eyes. The eyes are actual physical extensions of the brain. According to eye doctors, some binocular vision disabilities also involve problems with how the brain processes the visual information coming in through the eyes. Even so, many people with strabismus are offered only surgery to straighten the muscles of the eye. Surgery might make a deviating eye appear straight to others, but it often does very little to change the way the patient's brain processes incoming visual information. Often, the deviating eye returns to its misaligned position(s) after surgery. In other words, surgery frequently does not restore binocular vision.
Vision therapy (or orthoptic therapy) is a very effective type of physical therapy for the brain and the eyes. Children with binocular vision impairments can often learn to see normally by undergoing this type of rehabilitative therapy.
Consider the tremendous advances that have been made in the last forty years in the fields of occupational therapy and physical therapy. In these areas of therapy, health care professionals understand that the human brain is capable of tremendous change, recovery and development.
Today, patients who suffer strokes or other traumatic injuries to the brain and nervous system receive extensive rehabilitation. Therapeutic procedures (exercises) teach them how to coordinate movement--how to breathe, speak, and/or walk. In his speech at the 1996
Democratic convention, Christopher Reeve referred to the tremendous progress that has already been made in rehabilitative therapies. Today, he is wiggling his fingers and doing more than anyone thought possible!
Vision is such a vital sense. Why isn't the vision care/eye care field more progressive in general?
Why don't more eye care professionals take advantage of the marvelous gains that have been and are being made in the other rehabilitative therapies?
What is Depth Perception and Why Do We Need It?
DEPTH PERCEPTION: an important aspect of normal, healthy vision; a result of good stereoscopic vision; the ability to visually perceive depth and three dimensional space; the ability to visually judge relative distances between objects; a perceptual skill that aids accurate movement in three-dimensional space.
You need depth perception because . . .
The web site of the American Academy of Ophthalmology stated in August, 1996: "many occupations are not open to people who have good vision in one eye only (that means no stereo vision, no binocular depth perception)"
Here are a few examples of occupations that depend heavily on stereo vision:
- Baseball player
- Waitress
- Driver
- Architect
- Surgeon
- Dentist
The loss of binocular depth perception robs a person of more than just the possibility of being a professional baseball player or dentist children-special-needs.org asserts that the lack of binocular vision is a serious vision impairment that deserves more attention. Loss of binocular vision decreases quality of life as well as life choices. Parents and patients need to be informed about early detection of these conditions as well as the full range of treatment options.
Here are a few examples of general actions that depend heavily on depth perception:
- Throwing, catching or hitting a ball
- Driving and parking a car
- Planning/building a three-dimensional object
- Threading a needle and sewing
- Reaching out to shake another person's hand
- Pouring into a container
- Stepping off a curb or step
Eye Muscle Surgery (Strabismus Surgery)
See an extensive eye surgery FAQ, written by Dr. Jeffrey Cooper, a specialist in amblyopia (lazy eye) and strabismus (deviating eyes).
You are also invited to visit visionstories.com to read comments from parents and patients regarding eye muscle surgery for lazy eye, esotropia, exotropia, crossed eyes, etc.
Various scientific studies report success rates for eye muscle surgeries ranging from 30% to 80%. One scientific research study (Flax and Duckman, Orthoptic Treatment of Strabismus, Journal of AOA, 49th edition (12) p. 1353, 1978) reported a 50% success rate only as a result of surgical treatment for strabismus. However, success was defined as ANY long-lasting positive benefit. That is, the case was counted as a success if the patient gained ONLY a cosmetic improvement (the eye appeared more straight to others), but had no improvement in visual function (the ability to use both eyes to see normally).
Here at children-special-needs.org, we hear from parents of children who have had disappointing results following eye muscle surgery. Surgery on the eye muscles failed to restore binocular vision and, in many cases, did not even produce lasting cosmetic improvement (the eyes still didn't look "straight" or the wandering eye went astray once again).
We hope that all patients will be informed that one strabismus surgery often leads to another. Before consenting to the first eye muscle surgery, ask the eye surgeon if multiple surgeries might be recommended.
...from one of our visitors:
"I just finished watching one of my favorite shows, 'The Operation' on the Learning Channel. Tonight's operation was on a 17-year-old cross-eyed girl. It was her FIFTH eye surgery! After every previous surgery her eyes had eventually reverted to the crossed position. Watching this program prompted me to jump online and get some strabismus information."
Patricia S. Lewis
Read what Dr. Donald Getz, a specialist in the treatment of strabismus and lazy eye, says on the subject of surgery as compared to Vision Therapy.
References to some existing studies on eye muscle surgery are published on ourReferences page.
Can My Child Outgrow His Problem?
www.children-special-needs.org has communicated with parents of children who were told by pediatricians, teachers, pediatric ophthalmologists or pediatric optometrists that their child will "grow out" of his or her binocular vision impairment.
The following is a quote by Dr. Donald Getz, specialist in the treatment of strabismus and lazy eye. Dr. Getz comments on the mistaken notion that children will grow out of crossed-eyes and other binocular vision problems.
"THERE ARE MANY ALTERNATIVES to be considered in deciding the treatment program for patients with strabismus and amblyopia. The first alternative to be considered is what is likely to happen if nothing is done. Many patients have been advised by well-meaning doctors, friends and relatives that the child might grow out of the problem. This is practically never the case. Unless remediation is attempted, the problem will either remain the same, become more deeply imbedded, or adaptations will take place which will make Vision Therapy at a later date either more difficult or, perhaps, even impossible to conclude successfully. The child simply does NOT grow out of the problem." Dr. Donald Getz